In 2015, my first child had a terrible experience with Jaundice treatment – a total of 11 blood tests before proving she is OK!
Things have changed since 2018, and I got another chance to experience it again with Jade, my 2nd child.
UPDATE: On Day 42, after 5 blood tests, Jade is finally discharged.
What’s new in 2018?
Singapore first national guideline was established in Oct 2018 (PDF). What took them so long.
The biggest difference is the use of a device to measure bilirubin levels, without drawing blood. Hurray!

Transcutaneous Bilirubin (TcB) Measurements works by
directing light into the skin of a neonate and measuring the intensity of the specific wavelength that is returned.
The main goal of TcB measurement is to reduce the number of invasive blood tests required.
But the device is less accurate than blood test, so they apply 80% discount to the threshold.
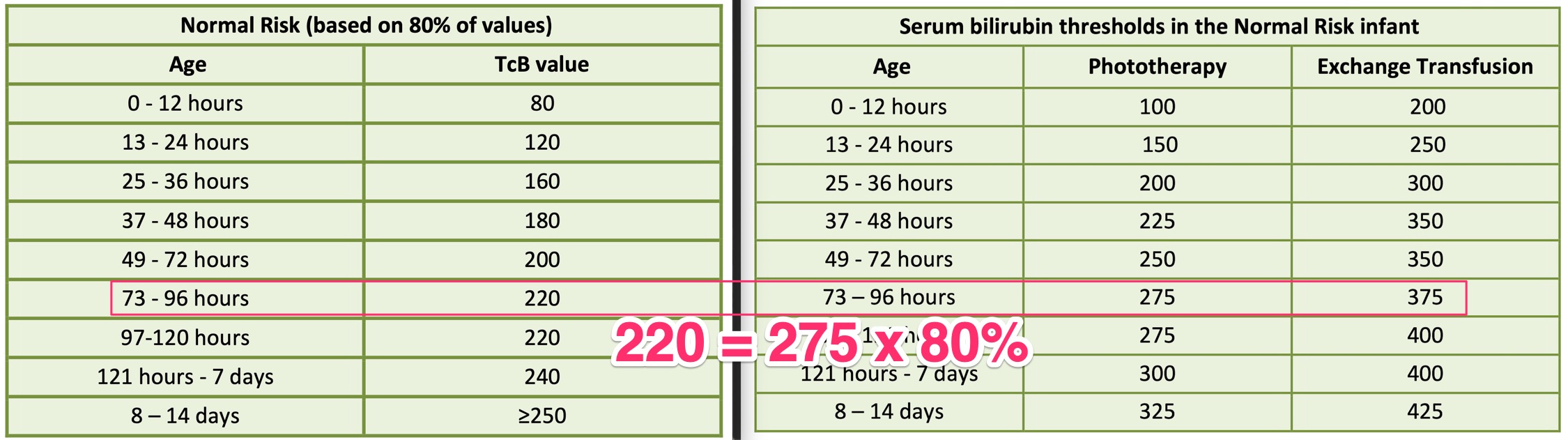
I took my child to the polyclinic on day 4, so she is 73-96 hours, as highlighted in that row. Her TcB measurement is 230, exceeding the 220 threshold. If TcB exceeds, then accurate blood test is needed.
Therefore she needs a blood test! Bloody hell..
The blood test came out as 253, which is lesser than the 275 threshold (a good news), therefore she doesn’t need phototherapy.
Compared to other country’s threshold, Singapore sets at 275 while America sets at 308 – that’s 10% more kiasu/kiasi.
The doctor advise us to come the next day to be measured again. This was like 5 years ago, when my first child took 11 blood tests!
Quoting from the guideline
The guideline gives good introduction to jaundice, including mentioning a brief history of Singapore olden days:
In 1960s, for 4 decades, neonatology units in local restructured hospitals have monitored affected newborns for 14 to 21 days after birth… the duration of hospitalisation has been cautiously reduced to 7 days from early 2000 and currently to the first 3 days.
Protocols change as we understand better.
Approximately 60% of term neonates and 85% of preterm neonates will develop jaundice, mostly as physiological jaundice which is usually benign.
Jaundice is very common.
I strongly believe we will further improve the guideline, given a few more decades, or wait till I’m a grandfather..
Likely Harmless Jaundice
Physiological jaundice is harmless, and they go away. It took 1 month for my first child.
Quoting the guideline on this physiological jaundice:
- often appears 2 - 3 days after birth
- serum bilirubin (SB) level rises to a peak of 105 – 140 μmol/L by day 3 to 5 in most full-term infants
- level up to 205 μmol/L is not uncommon
- often resolves in the first two weeks
Oh, Chinese race also has a significantly higher factor of getting jaundice, at 1.64x!
Normal Risk
Another important factor to consider is that my baby is NOT high risk.
High risk infants include preterm, low birth weight, inadequate breast feeding.
No symptom
Also, my baby does not show any of the clinical signs:
lethargy, poor suck, hypotonia, and high pitched cry
How I handle this time..
The blood test result is 253, and the doctor wanted us to return for another test the next day.
I am sure if we return the next day, it will be high, just like 5 years ago. And I gave myself good advise 5 years ago.
Repeated blood tests are huge waste of blood and time. Take doctor’s advice and make your own judgement. For example: If the level is 200, and doctor ask you to come the next day, it is unlikely it will go down to level 100 over night. So.. don’t do unnecessary blood test.
With past experience, we (including my wife who usually worry about every little thing) have cooly decided to NOT follow up on the next-day appointment. 😎
We shall not visit the polyclinic, unless she shows any symptoms, or I can see that she turned even more yellowish.
As quoted in the guideline, it is OK to use your eye to “see jaundice”. And I do have experience with identifying jaundice. 🤓
Visual inspection of baby for jaundice should be done preferably in natural light.